The impact of software on decision-making in oncology
Posted on 7 April 2017
The impact of software on decision-making in oncology
 By Jakob Nikolas Kather, MD, MSc, National Center for Tumor Diseases (NCT), Heidelberg, Germany.
By Jakob Nikolas Kather, MD, MSc, National Center for Tumor Diseases (NCT), Heidelberg, Germany.
This article is part of our series: A day in the software life, in which researchers from all disciplines discuss the tools that make their research possible.
Diagnosis and treatments in oncology
Cancer is a common disease and one of the leading causes of death. If detected at an early stage, some types of cancer can be cured by surgery, but often a tumour is detected at an advanced stage, and its cells have already spread throughout the body. Although many of these patients cannot be completely healed, several different treatment options are available. These treatments make a difference for cancer patients: they can significantly prolong life and often reduce symptoms as well. For each patient, we face the question: which treatment option is optimal at the current point of the disease? Clinical trials in the last decades are providing us with guidance in many situations. Often, there is an established "state of the art" for a treatment that has been shown to be superior to other options. However, as the arsenal of treatment options keeps growing, it is increasingly difficult to compare all options under all circumstances. Also, on the other hand, novel and more sophisticated diagnostic methods yield an ever-growing amount of data to base treatment decision on. For example, a patient with a newly diagnosed metastatic tumour disease might present herself at an oncology centre with several computed tomography (CT) and magnetic resonance imaging (MRI) studies, extensive laboratory tests, genetic tests and an ample clinical history with several pre-existing diseases.
Software helps to make the right decisions
To integrate all this diagnostic information into one decision is often hard, if not impossible. Formally speaking, the oncologist has to consider an extremely high-dimensional parameter space where each patient resides at one point in a vast set of possible combinations. In particular, two problems arise: 1) Diagnostic information is not directly accessible to human observers. Visualisation has to be used to make the raw data intelligible to humans. For example, raw data from MRI studies has to be reconstructed as images so that humans can visually understand this information. 2) Even if a human observer has a good mental representation of all diagnostic information, it is hard (or impossible) to derive the optimal treatment decision from this. In both cases, software can help human oncologists and patients to make better treatment decisions.
Software helps to make data intelligible
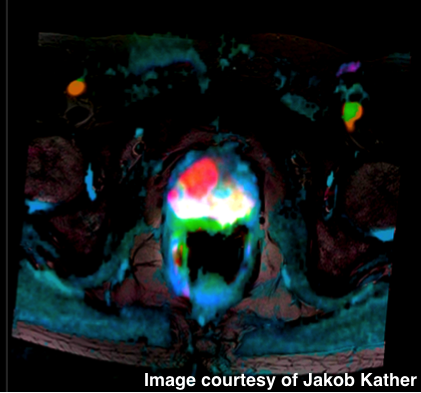
For many years, computer-based visualisation of diagnostic information has been crucial in oncology. For example, MRI yields information about tissue properties in a very abstract manner. Essentially, these effects are governed by quantum mechanics and the data, in their raw format, are completely unintelligible for humans. It is only through the use of software which reconstructs spatial information and then visualises this information that the data becomes accessible to human interpretation. A conventional visualisation of MRI data is shown in the left panel of Figure 1. Recently, we have developed a new method (Link: http://dx.doi.org/10.1038/srep41107) to visualise even more information in a single image in a way that humans can easily understand (Figure 1, right panel).
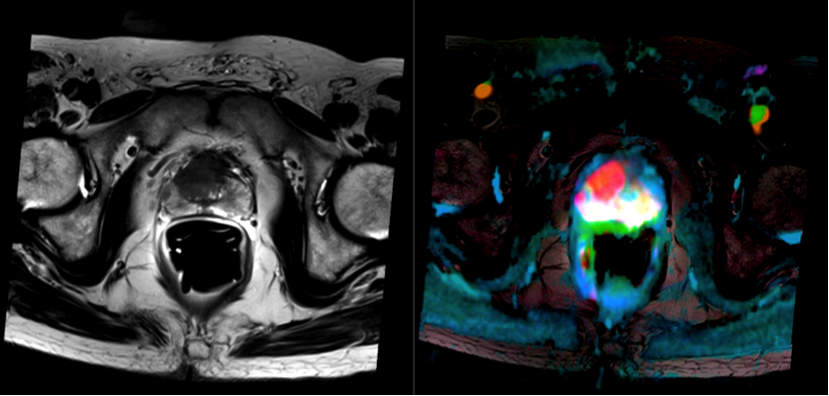 Figure 1: (Left) An MRI study of human prostate cancer. One channel is conventionally visualised (in grayscale). (Right) A new visualization of multiple channels of MRI data. The tumor lights up as a red patch in the prostate.
Figure 1: (Left) An MRI study of human prostate cancer. One channel is conventionally visualised (in grayscale). (Right) A new visualization of multiple channels of MRI data. The tumor lights up as a red patch in the prostate.More data makes decisions harder
Assume that a human observer has a perfect mental representation of all available data. Is it easily possible to derive a meaningful decision from this data (in our case: which therapy to employ)? Clearly, this is not the case. With an increasing amount of data, it becomes much harder to draw an optimal conclusion. Not surprisingly, for most clinical decisions, only a handful of up to a dozen parameters are used. But as ten binary variables can be combined in 2^10 different ways, this already yields an enormous decision space (or a very large decision tree). This is visualised in Figure 2 for three independent variables.
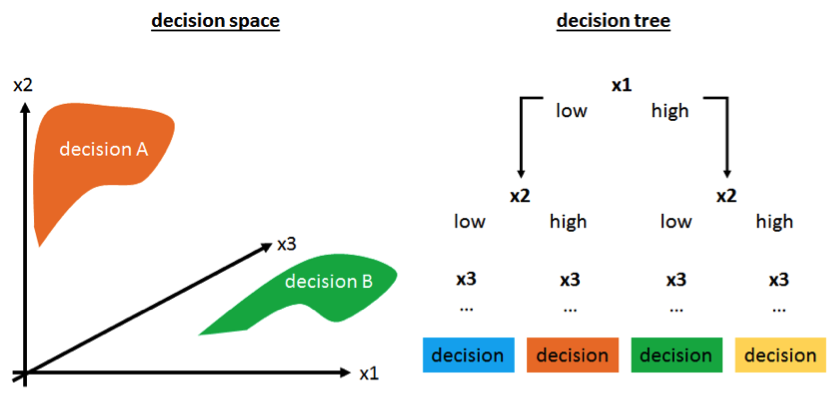 Figure 2: High-dimensional decision making visualised as a decision space (left) or a decision tree (right).
Figure 2: High-dimensional decision making visualised as a decision space (left) or a decision tree (right).Software can aid treatment decisions
In these types of decision problems, software can help humans, as it can aggregate several measurements into a single risk score that can be more easily understood. For example, for breast cancer, several commercially available assays yield a risk score based on some dozens of genes. For a human observer, this simplifies decision making as the complexity of the problem diminishes. On the other hand, information might also be lost in this process, and it is hard to validate a new risk score.
Summary
Optimal decision-making in oncology is very important for patient wellbeing. As the availability of diagnostic information increases, this decision-making process is getting harder. One reason is that humans cannot mentally understand all available information. The other reason is that the decision space (or decision tree) becomes so complex that humans cannot easily navigate here. In both cases, software can make an important contribution and facilitate decision-making.
